Brain connectivity in a dish
Schizophrenia is thought to arise from disrupted neural connections in the brain. Recent evidence derived from magnetic resonance imaging (MRI) studies provides clear support for this hypothesis. However, interpretation of MRI data is limited due to poor spatial resolution; MRI techniques in isolation cannot capture specific biological mechanisms.
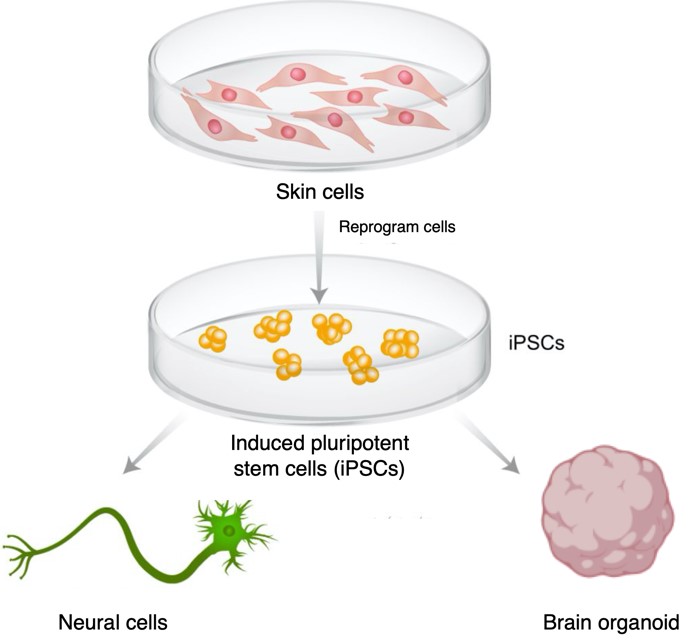
Cutting-edge stem cell technologies provide new avenues to explore connectivity disruptions in schizophrenia. Induced pluripotent stem cells (iPSCs) can be reprogrammed from human (blood/skin) cells obtained from individuals with schizophrenia. IPSCs can be converted into neural cells and mini brains (organoids) to study disease mechanisms “in a dish” (see figure for an overview of this process).
The overall purpose of this project is to integrate MRI findings with cellular disease models of schizophrenia. This project will be supervised across two departments at the University of Melbourne: Department of Psychiatry and Department of Anatomy and Physiology.
Further research and key questions
- Develop and improve methods to model neural connectivity in vitro
- Identify cellular links to large-scale brain imaging findings in schizophrenia
Project leaders
Maria Di Biase, Maciej Daniszewski, Alice Pebay
Further reading
- Di Biase MA, Pantelis C, Zalesky, A. White Matter Pathology in Schizophrenia. In Neuroimaging in Schizophrenia (pp. 71-91). Springer, Cham.
- Hoffmann A, Ziller M, Spengler D. Progress in iPSC-Based Modeling of Psychiatric Disorders. Int J Mol Sci. 2019;20(19):4896.